Arthritis is a leading cause of pain and disability worldwide. In the United States alone, arthritis affects 50 million adults and over 300,000 children. Arthritis is not a single diagnosis, but in fact a collection of conditions that causes pain and aches related to joint paint.
Arthritis comes in a variety of forms and affects people differently – but the most common types are osteoarthritis and rheumatoid arthritis. And while over-the-counter medications and prescriptions can be effective, many patients do not want to take the risk of taking medication. There are many alternative methods for arthritis treatments that do not include taking pills or utilizing a prescription.
Finding Relief from Arthritis Pain
Treatments for Arthritis Pain Relief
-
The Right Pair of Shoes
According to a study, researchers found that in people with osteoarthritis, flexible shoes like flip-flops and sneakers reduce the force exerted on knee joints by an average of 13% compared to clogs and specialty shoes.
More force on joints equates more pain, so if by wearing flexible shoes there is less force, it should mean there is less pain. This is best to relieve pain in those who suffer from osteoarthritis of the knee and hip.
2. Aquatic Exercises
Water provides a resistance that increases the intensity of an exercise while also providing buoyancy that supports your bodyweight and relieving pressure on your joints.
Water aerobics and exercises have been proven to help improve range of motion, coordination, quality of life, and reduce body fat. While it may not be a long-term solution, patients who participate in aquatic exercises find relief from arthritis pain.
3. Yoga
Yoga, specifically Iyengar yoga that focuses on proper body alignment to support the body and relieve tension, is an excellent way to help relieve arthritis pain. Yoga is helpful in patients with rheumatoid arthritis in relieving pain, improving mood, and the ability to cope with their chronic arthritis pain.
- Supplements
Natural supplements are regularly being researched and approved for help in relieving pain associated with arthritis. Many supplements have properties that act as natural anti-inflammatories and the ability to stimulate neurotransmitters, like serotonin, which reduce pain receptors. Some supplements include:
- Indian Frankincense
- Tumeric
- Fish Oil / Omega 3
- Ginger
5. Massage
Regular massages help relieve tension and relax muscles and joints. Professional massages lower the body’s production of cortisol (the body’s stress hormone) and the neurotransmitter substance P, which is associated with pain. Massages help improve patients’ moods by boosting serotonin levels.
6. Therapy
Different kinds of therapy – exercise, physical, and cognitive behavioral therapies – are all beneficial to patients who suffer from arthritis pain. It improves your body’s strength, posture, range of motion, and functionality. Exercise is known to improve your mood, and when used in conjunction with cognitive behavioral therapy (CBT) it can be incredibly helpful in reducing pain.
CBT, or talk therapy, helps you identify pain points and makes you more aware of the anxieties and stress that is often associated with types of chronic pain like arthritis.
7. Sleep
Giving your body time to rest and relax at night is one of the most effective ways for it to heal and be free from pain. However, if you suffer from chronic pain, then you know that sleep is often disturbed and unachievable. Sleep deprivation can make pain worse and negatively affect your overall health.
Developing a strict schedule, setting alarms when it’s time to wake up and go to bed, help your body’s internal clock and help “reset” your natural sleep cycle. Napping disrupts the cycle, as well as trying to “catch up” on sleep on the weekends.
Being more active during the day can not only help reduce pain, but it will tire you out and make falling asleep easier. Studies have shown that patients who get seven or more hours of sleep a night are happier and healthier.
Arthritis can affect people in many different ways. If you experience any problems or have concerns about using at-home arthritis treatments, talk to your doctor. If you are currently taking medication for your arthritis pain, speak to your doctor before taking any supplements or undergoing any type of therapy for safety purposes.
If you suffer from sciatica, you know how painful it can be. It disrupts your daily life, affecting everything from sitting in the car to standing in the kitchen to make a meal.
Sciatica is a term used for any pain or symptom that causes numbness or sensation like tingling along the sciatic nerve. This means sciatic nerve pain isn’t a true diagnosis but a description of the pain you are experiencing that can help doctors properly assess your pain to determine a source.

Types of Sciatic Nerve Pain
The sciatic nerve runs from your lower back through your hips and down each leg. Generally, when a patient experiences sciatica, it only affects one side of the body.
Common Causes of Sciatic Nerve Pain
Most commonly, sciatica is caused by a herniated disc. Although other lower back conditions can attribute to sciatic nerve pain: arthritis, spinal stenosis, and spondylolisthesis. Sciatica can also be painful if there is a pinched nerve from a bone spur or tumor that is pressing on the nerve.
Types of Sciatic Nerve Inflammation and Pain
Neurogenic
Neurogenic sciatica is caused by compression of the sciatic nerve, caused by a number of things, such as bulging discs to tight muscles. The discs can bulge, herniate, or burst, and this causes pressure on the nerves along the spine. Direct pressure on the spinal cord also compresses the sciatic nerve, as well as tight muscles from the buttocks and upper thigh.
Typically, pain is worse in the leg than in the back. Symptoms vary depending on how severe the pressure is, but the pain can be described as sharp, shooting, and even burning pain. It’s common to experience numbness, hot and cold sensations, muscle weakness, and tingling.
This type of sciatic nerve pain is associated with abnormal neurological exam findings like loss of normal reflexes, sensory changes, and muscle weakness.
Referred
Referred pain is caused by a muscle or joint problem in the spine or pelvis. It is not truly a form of sciatica but mirrors the pain and symptoms. It is important to determine the cause of the pain. This type of sciatic nerve pain is usually dull and achy, not usually giving off a sensation of pins and needles.
This type of pain is not caused by a pinched nerve, but by a sprain or strained joints and muscles.
Risk Factors for Sciatica
There are multiple reasons you may experience sciatica, including:
-
- Age: age-related changes in the spine can cause bone spurs and compressed nerves
- Obesity: Excessive body weight can cause extra weight and pressure on the spine and trigger spinal changes that cause sciatica.
- Diabetes: Fluctuating blood sugar increases your risk for nerve damage.
- Long Periods of Sitting: People who have sedentary lifestyles are much more likely to develop sciatica than active people.
Preventing Sciatic Nerve Inflammation
While sciatica may not be completely avoidable, there are certain ways to protect your back from recurring pain:
- Regular Exercise: Keeping your back strong and paying attention to core strength in the abdomen and lower back are essential for proper alignment.
- Maintain Good Posture When You Sit: Sitting with lower back support, armrests, and a swivel base help your posture. Keep you knees and hips level, and consider adding a small pillow in the small of your back to maintain its normal curve.
- Be Mindful of Good Body Mechanics: Be mindful of your body while doing regular daily activities and if you do physical labor for work. If you stand for a long time, alternate propping your feet up on a small box from time to time. When lifting something heavy, use your knees instead of relying on your back – keep your back straight and bend at the knees. Get help lifting large items so you don’t stress your muscles or joints.
Pain does have a purpose, although it can be uncomfortable. When pain overstays its welcome, it can alter your quality of life and prevent you from living your best life.
Chronic pain can be debilitating and for patients who have suffered for years with pain and discomfort, they may not be interested in undergoing perhaps another surgery or trying a new pain medication. Patients who have chronic pain just want relief and to restore a sense of normalcy to their lives.

Learn how to manage your pain on a daily basis
Thanks to extensive research and the evolving field of pain management, there are more options than ever for effectively managing chronic pain on a daily basis, whether at home or on-the-go. Many of these options are natural remedies and can effectively help reduce pain without taking medications.
Ways to Manage Pain on a Daily Basis
- Hot and Cold Compress
Two tried-and-true methods, these are still a great foundation for relieving pain at home. A cold compress can be used to relieve pain, decrease inflammation, and reduce muscle spasms. Heat increases your pain threshold and relaxes muscles. If a homemade ice or heat pack don’t do the trick, as your physician for advice or versions of this treatment method. They may be able to suggest a device or way to apply heat or ice that penetrates deeper into your muscles.
- Therapeutic Massages
While massages can be an indulgence and be very relaxing, they can be very helpful to those in pain. Massages work tension out of muscles and joints and relieve stress and anxieties. Massages often produce a “competing” sensation that is more powerful than pain signals and distracts you from the pain you experience.
- Yoga
Yoga affects all aspects of the body: physical, emotional, spiritual, and vital. The yoga postures (asanas) and breathing aspects (pranayama) affect the psyciological system and trigger a “relaxation response” in the neuroendocrinal system. What this means is that yoga can decrease metabolism, stable blood pressure, reduce muscle tension, and diminish fatigue. Additionally, yoga can help reduce anxiety and stress from coping with chronic pain.
- Biofeedback
Biofeedback combines relaxation techniques with breathing exercises in conjunction with a biofeedback machine. This machine creates data from heart rate and blood pressure into visuals like a graph or animation. Watching that animation gives you a sense of control over your body’s responses to pain.
To say that COVID-19 has thrown a wrench into our daily lives would be a massive understatement. As pain management professionals, we had to quickly adapt to the challenges this pandemic put in front of us and navigate a new landscape of twists and turns while continuing to provide top-notch healthcare to our patients.
Telemedicine for Pain Management in NJ

Telemedicine for Pain Management in NJ
One of the most significant changes the COVID-19 pandemic has brought about is the way we meet with others. Video conferences have replaced in-person meetings in the workplace, and the same holds true in the healthcare industry. Thanks to technology, we were able to transition smoothly to a telemedicine-based approach, whenever appropriate.
Telemedicine allows us to communicate with our patients while minimizing the risk of infection. Chronic pain doesn’t stop for a pandemic, so video chats and phone calls allow us to provide the same level of healthcare without putting our patients or employees at risk.
Some of the things we can utilize telemedicine for include:
- Initial Consultations
- Prescription Refills
- Follow-up Appointments
Beyond minimizing the risk for infection, telemedicine came with other added benefits, including:
- Eliminating the need for travel for our patients
- Increased efficiency for our practice
- Ability to assess our patients in their home environment
- Ability to work with patients outside of our immediate geographical area
There are certainly procedures and situations that require us to meet with our patients face to face, and we take appropriate safety precautions in those cases.
If you are interested in telemedicine for your pain management, contact us today here.
COVID-19 Vaccinations and Steroid Injections

Covid-19 Vaccinations and Steroid Injections
With the emergence of the Pfizer, Moderna and Johnson & Johnson COVID-19 vaccines, we need to be mindful when scheduling steroid injections for chronic pain relief. While there is no data to support negative interactions between steroid injections and COVID-19 vaccine administration, it is accepted as a general rule of thumb to wait 2 weeks before and 2 weeks after the administration of the vaccine before receiving any steroid injections.
Since there is no long-term data yet on COVID-19 vaccines, the 2-week waiting window is derived from guidance on other existing vaccines. While there hasn’t been any evidence of immunity suppression from the steroid injections, it’s better to err on the side of caution until we have enough data on the subject.
Pain Management in COVID-19 “Long Haulers”
COVID-19 survivors may be at risk of opiate addiction, due to the high rate of pain medications being prescribed while recovering from the virus. While hospitalized, these patients may be prescribed opiates such as OxyContin, Vicodin or Codeine for their pain or anxiety. For example, patients put on ventilators to assist with breathing, may be sedated in order to remain comfortable.
This puts a whole new group at risk for future opiate dependency without the proper guidance from an experienced pain management doctor.
Alternative treatments such as physical therapy, over the counter anti-inflammatory medication or biofeedback may be recommended for long haulers in lieu of opiates.
These are just a few of the ways pain management healthcare has changed in the face of COVID-19. While we continue to face new challenges as variants of the virus emerge, you can always count on Progressive Pain Management to evolve and adapt. Our goal is to provide our patients with the best pain management throughout New Jersey!
100 adult patients suffering from chronic, severe nonmalignant pain were studied over the course of 12 months by Anjum Bux, MD, director of chronic pain management at Ephraim McDowell Regional Medical Center and Harrison Memorial Hospital in Danville and Cynthiana, Ky. The criteria for the 100 individuals required they have already undergone 6 months of conventional pain management prior to the introduction of an intrathecal pump.
What is an Intrathecal Pump and How Does it Help with Chronic Pain Management?

An intrathecal pump is implanted under the skin in that abdomen and delivers medication directly to the spine.
An intrathecal pump is a device that is used to deliver pain medication such as morphine, ziconotide and baclofen directly to the spinal cord. The small pump is surgically implanted beneath the skin, usually in the abdomen, and uses a catheter to deliver pain medication to the appropriate region.
Intrathecal pumps are often used to treat conditions such as chronic back pain, chronic neck pain or sciatica. Some patients suffering from failed back or neck surgery may also benefit through the use of an intrathecal pump for. The pump can often replace administration of oral opioid medications in chronic noncancer pain patients.
There are two main styles of intrathecal pumps – fixed rate and variable rate.
- Fixed rate pumps – mechanically operated and no battery required.
- Variable rate pumps – contain a battery and integrated circuitry which allow rate of delivery to be adjusted. Variable rate pumps may need to be replaced over time due to the use of a battery
Measuring the Effectiveness of Medication Delivery Via an Intrahelical Pump
![]() The study tracked a variety of primary outcomes:
The study tracked a variety of primary outcomes:
- Changes in mean visual analog scale (VAS) pain scores
- Morphine milligram equivalent usage
- Number of daily medications
- Number of daily narcotics
The following secondary outcomes were also tracked:
- Changes in the number of ER visits
- Non–health care–related visits
- Number of hospitalizations.
Results of Study Show Significant Benefits When Using Intrathecal Pump
Bux reported a significant drop in mean VAS scores in the 100 participants after switching to the use of an intrathecal pump. VAS scores dropped from 7.81 to 5.81 (P<0.001).
The study also showed a drastic change in the use of daily oral or transdermal morphine equivalents. These dropped from 57.89 to 2.91 mg (P<0.001). The number of pain medications consumed by the participants also dropped from 1.78 to 0.98 (P<0.001).
The secondary outcomes tracked in this study also supported the case for intrathecal pumps.
- Hospitalizations – 0.22 to zero (P<0.001)
- Non-pump-related clinic visits – 0.81 to 0.53
- ER visits – 0.69 to 0.54
Bux concluded that the use of an intrathecal pain pump led to better pain control, as well as decreases in amount of total medications, narcotics, pain medications and ER visits.
Are you a candidate?
 Do you think you or a loved one may be a candidate for an intrathecal pump for pain management? Contact Progressive Pain Management today. We have 3 offices located conveniently throughout New Jersey.
Do you think you or a loved one may be a candidate for an intrathecal pump for pain management? Contact Progressive Pain Management today. We have 3 offices located conveniently throughout New Jersey.
Ocean Township Pain Management
References:
painmedicinenews.com (Account required to read full article)

Endoscopic rhizotomy may be the key to your chronic back pain relief.
In a study published December 2014, a common treatment for back pain known as conventional fluoroscopically guided continuous radiofrequency (CRF) and pulsed radio frequency (PRF) is compared to an endoscopic visually guided method.
A specially designed cannula and endoscope were developed specifically for this visualized, surgically directed endoscopic technique. The instruments were designed ergonomically, to keep the image in focus while the endoscope scope is resting on the cannula.
The technique used in this study allows the doctor to ablate a larger area of the transverse process where the medial branch crosses to innervate the facet. Nerve ablation or transection can be confirmed via endoscopically guided visualization.
The Method used in This Chronic Back Pain Study
The efficacy of endoscopic rhizotomy was initially evaluated through a retrospective non randomized study of 50 patients (originally carried out in 2005). The requirements for patients to be candidates for the surgically directed endoscopic technique were as follows:
- Patient had lumbar spondylosis and facet arthrosis
- Patient experienced at least 50% pain relief by medial branch blocks
Cadavers aided in surgical technique refinement. Cadaver dissections showed variations in the locations of the dorsal ramus, including the medial branch. These anatomic variations clearly demonstrated the benefits of visualized rhizotomy
Once efficacy was demonstrated in this initial study, 400 more patients were added to this retrospective study by May 2013. It was at this time the inclusion requirements were boosted to a base of 75% estimated improvement. This was done to circumvent the variable subjectiveness of a 50% improvement threshold. This minimized the possibility a patient may be overestimating their initial response to treatment in hopes that they would qualify for the endoscopic guided procedure.
Endoscopic Rhizotomy Study Results
Patients were evaluated one year after the study design. All patients had VAS (visual analog scale for pain) improvement equal or greater than injection. The results of this chronic back pain study aligned with findings in additional surgical cases. Greater surgical exploration could be achieved by using visualized rhizotomy, resulting in a higher level of back pain relief for patients. Approximately 10 percent of the patients had mild recurrence of their back pain when following up one and two years later, but none to the original level of pain.
Continuous Radiofrequency (CRF) and Pulsed Radiofrequency (PRF) Study
CRF and PRF are common treatments for chronic back pain. While these methods are commonly used, even when successful, the relief provided by this form of treatment is usually temporary.
In 2005, a non-randomized retrospective study was carried out to assess the effect of endoscopic radiofrequency lesioning in 50 patients with chronic back pain. Patients were required to experience at least a 50% improvement in pain utilizing medial branch blocks to qualify for the study.
As time went on, the requirements to participate in the study became more stringent to further restrict the recommendation for surgical intervention. By 2013 the study size grew to 450.
Results of CRF / PRF Study
Out of the 50 original participants of the study, 10 percent partially regressed at the one-year follow-up, but none were worse. All patients were glad to receive the rhizotomy treatment, even if some of the pain relief had already begun to fade a year later. All patients experienced relief of back pain equal or greater than they had prior to the intervention, and some had relief of sciatica as well.
As time went on and treatment as given to the remaining 400 participants, the procedure evolved and became more effective. Further review of cadaver anatomy led to the second phase of the study, where inclusion criteria was adjusted to maximize the potential for positive results.
Conclusion
The results of those chronic back pain studies suggest that endoscopic rhizotomy targeting the variable dorsal ramus anatomy is more effective and provides longer lasting results than the traditional fluoroscopically guided procedures. The inclusion of an endoscope helped bridge the gap between open surgical procedures and traditional pain management techniques, while providing a minimally invasive surgical option to maximize the potential for longer lasting pain relief.
References:
You can learn more about these studies by visiting: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4325504/
 A spinal cord stimulator (SCS), also known as a dorsal column stimulator, is a device surgically placed under your skin to send a mild electric current to your spinal cord. This therapy can essentially reduce your pain significantly.
A spinal cord stimulator (SCS), also known as a dorsal column stimulator, is a device surgically placed under your skin to send a mild electric current to your spinal cord. This therapy can essentially reduce your pain significantly.
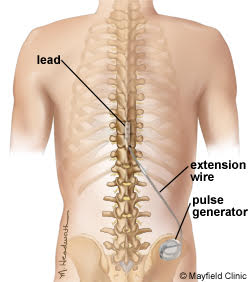
Stimulation does not eliminate the source of pain, it simply interferes with the signal to the brain, therefore, the amount of pain relief varies for each person. The device is first done as a trial before it is placed permanently. The goal for spinal cord stimulation is a 50-70% reduction in pain. However, even a small amount of pain reduction can be significant if it provides you with quality of life and a decrease or elimination of your pain medications.
If the trial is unsuccessful, the implant can be removed and does not damage the spinal cord or change the anatomy.
FDA-approved indications include the following:
1) Failed Back Surgery Syndrome (FBSS)
2) Chronic painful peripheral neuropathy
3) Multiple Sclerosis (MS)
4) Complex Regional Pain Syndrome (CRPS) I and II
You may be a candidate for SCS if you meet the following criteria:
*This procedure is performed by Dr. Bannister as an outpatient procedure and is covered by insurance.
Stem cell therapy is a natural way of treating conditions such as knee pain, shoulder pain and hip pain. This is a minimally invasive, out patient procedure that is performed by Dr. Bannister.

How it Works:
Chronic joint pain is usually due to degenerative changes of the bone and soft tissue within the joint. Stem cells have been shown to regenerate the tissue that has been lost due to normal wear and tear.
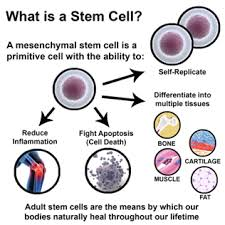
How it’s Done:
Stem cells are harvested from your bone marrow or adipose tissue (usually the abdomen). The cells are then processed and injected into your problem area. Mature stem cells reproduce quickly and can repair damaged joints.
Discomfort should be minimal, with some localized pain around the injection site.
Stem Cell Therapy is not currently covered by medical insurance.
 Treatment for lower back pain depends upon the patient’s history and the type and severity of pain. The majority of lower back pain cases get better within six weeks without surgery.
Treatment for lower back pain depends upon the patient’s history and the type and severity of pain. The majority of lower back pain cases get better within six weeks without surgery.
Examples of conservative treatment includes:
– Rest, Ice and or heat
– Exercise, Physical Therapy and Chiropractic treatment
– Medications (OTC or prescribed)
If you continue to have pain despite conservative treatment and you have any of the following diagnoses, we can offer you minimally invasive treatment options:
– Low back pain
– Sciatica
– Spondylolisthesis
– Sacroiliac Joint Dysfunction
– Spinal Stenosis
– Degenerative Disc Disease
– Lumbar Facet Arthrosis
– Failed Back Surgery Syndrome
Treatment for the above conditions include:
– Lumbar Epidural (Translaminar vs. Transforaminal)
– Lumbar Facet Injections
– Dorsal Column Stimulator Therapy
– SI Joint Injections
– Radio Frequency Ablation (For Facet and SI joint problems)
– Laser Therapy
A facet rhizotomy injection is a minimally invasive procedure that attempts to relieve neck or back pain associated with facet disease by using an electrical current to ablate local nerve fibers that carry pain signals from the affected joint to the brain. This is performed as a same day, outpatient procedure.

An intrathecal pump is a medical device used to deliver medications directly into the space between the spinal cord and the protective sheath surrounding the spinal cord.
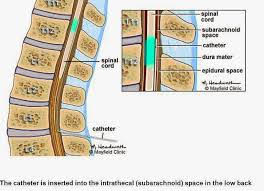
Delivery of drugs into spinal fluid requires smaller amounts of medication and is often more effective at controlling pain than oral therapy.
Spinal analgesia may be so effective, that patients are able to reduce or discontinue oral pain medications, thus decreasing associated side effects.
Who is a Candidate?
*This procedure is performed by Dr. Bannister in an outpatient setting and is covered by insurance.

